Health News
- Expert Says Ky. Is One Of 13 States Where People In Individual Insurance Market Are Better Off Than Before Reform Law
By Molly Burchett and Al Cross Kentucky Health News Most of the focus on Obamacare has been on people who are no longer uninsured, or those who had to get new policies, but Kentucky is one of the 13 states in which the Patient Protection and Affordable...
- Humana, United And Assurant Allow Non-compliant Policies To Be Extended; Anthem And Bluegrass Offer Sort Of Half A Loaf
Some health-insurance companies won't give Kentucky customers the opportunity to renew polices that don't comply with the federal health-reform law, under the conditional extension granted by President Obama, state Insurance Commissioner Sharon...
- Humana Allows Policyholders To Keep Old Plans Without Paying More; Anthem Is Still Deciding
Humana, one of the three insurance companies offering individual health policies on the state's insurance exchange, will allow Kentuckians to keep their insurance coverage for another year without charging them more for it. The other two companies...
- At Least One Insurance Company Will Let Kentuckians Keep Their Health Insurance Plan For Another Year If They Like It
By Molly Burchett Kentucky Health News At least one insurance company, Humana, will be allowing Kentuckians to keep their insurance coverage for another year if they like it, even if the policies aren't compliant with the Patient Protection and Affordable...
- Doi Moves To Allow Consumers To Continue Current Coverage Into 2014
The Illinois Department of Insurance (DOI) announced on November 22 that it will follow President Obama?s November 14 recommendation and allow insurance companies to renew a number of health plans in the individual and small group markets that do not...
Health News
280,000 Kentuckians, almost all those with individual and small-group insurance policies, will have to change under Obamacare
By Molly Burchett
Kentucky Health News
About 280,000 Kentuckians will have to give up their current insurance policies, which are being discontinued because they don't comply with the Patient Protection and Affordable Care Act, according to the state Department of Insurance.
Department spokeswoman Ronda Sloan said individual policies for about 130,000 people and small-group policies for about 150,000 more will be discontinued. This means that almost all Kentuckians in the individual (134,086) and small group (153,943) private insurance market segments will face policy discontinuation, requiring them to get different insurance coverage even if they like their current coverage.
 These Kentuckians join the millions of Americans who are getting or will get cancellation letters for their health insurance under Obamacare. An estimated 50 to 75 percent of the 14 million consumers who buy their insurance individually can expect to receive this type of letter over the next year because existing policies don?t meet the standards mandated by the health care law, reports NBC News.
These Kentuckians join the millions of Americans who are getting or will get cancellation letters for their health insurance under Obamacare. An estimated 50 to 75 percent of the 14 million consumers who buy their insurance individually can expect to receive this type of letter over the next year because existing policies don?t meet the standards mandated by the health care law, reports NBC News.
NBC says the Obama administration has known this would happen for three years, despite President Obama's statement that people who liked their health insurance would be able to keep it under the health law.
The plans that are being discontinued do not meet the requirements of the law, which standardized policies and set minimum standards. "This is not a ?cancellation? or a ?termination.? No one is losing coverage,? Sloan said in an email to The Associated Press. Discontinuation letters will offering a compliant plan that the consumer can switch to upon renewal, she said.
The consumer can also take this opportunity to shop around for other options through an insurance agent or on the state's Kynect website, where they may qualify for a subsidy or Medicaid coverage, Sloan noted. Kentuckians should be sure to purchase a plan that is from a licensed Kentucky company and is a qualified health plan, she said.
The health law requires all plans to offer 10 essential benefits, such as mental health care, prescription drug coverage and maternity and newborn care. Plans that don't cover such services typically have lower premiums.
In the small-group market, businesses can shop for employee coverage in the same way that individuals shop for coverage, through an insurance company, agent or Kynect.
Small employers have expressed concern about being able to afford coverage for their employees, citing rising premiums, and Sloan says there is no way for the Insurance Department to know whether or not an employer is planning to continue offering coverage to employees whose policies are being discontinued. "If not, those employees could purchase coverage on the individual market," she said.
After Humana Inc. sent discontinuation letters to 6,543 policyholders, the Insurance Department fined it $65,430 because the letters were misleading. They called for customers to renew their plans for 2014 within 30 days or choose a more expensive option that complies with the health law, and didn't clearly say that policyholders could compare and choose competing plans, for which they could possibly qualify for federal subsidies. In addition, they said that a customer could get the cheaper premium option by agreeing to changes not yet approved by the Insurance Department.
?The Department of Insurance fined Humana for providing members with a policy amendment form that was not approved. This was a clear-cut violation of Kentucky?s insurance code,? Insurance Commissioner Sharon Clark told Chris Kenning of The Courier-Journal.
State officials are also reviewing a letter sent by Anthem Blue Cross Blue Shield that asked people to "call now to lock in "today's affordable rates,", reports USA Today. The insurance department determined that the letter was marketing to potential customers, and thus did not violate the insurance code. "Humana?s letter, by contrast, went to current policyholders," Kenning reports.
Kentucky Health News
About 280,000 Kentuckians will have to give up their current insurance policies, which are being discontinued because they don't comply with the Patient Protection and Affordable Care Act, according to the state Department of Insurance.
Department spokeswoman Ronda Sloan said individual policies for about 130,000 people and small-group policies for about 150,000 more will be discontinued. This means that almost all Kentuckians in the individual (134,086) and small group (153,943) private insurance market segments will face policy discontinuation, requiring them to get different insurance coverage even if they like their current coverage.

NBC says the Obama administration has known this would happen for three years, despite President Obama's statement that people who liked their health insurance would be able to keep it under the health law.
The plans that are being discontinued do not meet the requirements of the law, which standardized policies and set minimum standards. "This is not a ?cancellation? or a ?termination.? No one is losing coverage,? Sloan said in an email to The Associated Press. Discontinuation letters will offering a compliant plan that the consumer can switch to upon renewal, she said.
The consumer can also take this opportunity to shop around for other options through an insurance agent or on the state's Kynect website, where they may qualify for a subsidy or Medicaid coverage, Sloan noted. Kentuckians should be sure to purchase a plan that is from a licensed Kentucky company and is a qualified health plan, she said.
The health law requires all plans to offer 10 essential benefits, such as mental health care, prescription drug coverage and maternity and newborn care. Plans that don't cover such services typically have lower premiums.
In the small-group market, businesses can shop for employee coverage in the same way that individuals shop for coverage, through an insurance company, agent or Kynect.
Small employers have expressed concern about being able to afford coverage for their employees, citing rising premiums, and Sloan says there is no way for the Insurance Department to know whether or not an employer is planning to continue offering coverage to employees whose policies are being discontinued. "If not, those employees could purchase coverage on the individual market," she said.
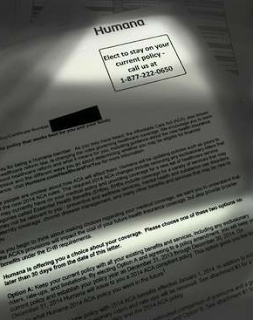 |
| Humana's misleading letter to policyholders |
?The Department of Insurance fined Humana for providing members with a policy amendment form that was not approved. This was a clear-cut violation of Kentucky?s insurance code,? Insurance Commissioner Sharon Clark told Chris Kenning of The Courier-Journal.
State officials are also reviewing a letter sent by Anthem Blue Cross Blue Shield that asked people to "call now to lock in "today's affordable rates,", reports USA Today. The insurance department determined that the letter was marketing to potential customers, and thus did not violate the insurance code. "Humana?s letter, by contrast, went to current policyholders," Kenning reports.
- Expert Says Ky. Is One Of 13 States Where People In Individual Insurance Market Are Better Off Than Before Reform Law
By Molly Burchett and Al Cross Kentucky Health News Most of the focus on Obamacare has been on people who are no longer uninsured, or those who had to get new policies, but Kentucky is one of the 13 states in which the Patient Protection and Affordable...
- Humana, United And Assurant Allow Non-compliant Policies To Be Extended; Anthem And Bluegrass Offer Sort Of Half A Loaf
Some health-insurance companies won't give Kentucky customers the opportunity to renew polices that don't comply with the federal health-reform law, under the conditional extension granted by President Obama, state Insurance Commissioner Sharon...
- Humana Allows Policyholders To Keep Old Plans Without Paying More; Anthem Is Still Deciding
Humana, one of the three insurance companies offering individual health policies on the state's insurance exchange, will allow Kentuckians to keep their insurance coverage for another year without charging them more for it. The other two companies...
- At Least One Insurance Company Will Let Kentuckians Keep Their Health Insurance Plan For Another Year If They Like It
By Molly Burchett Kentucky Health News At least one insurance company, Humana, will be allowing Kentuckians to keep their insurance coverage for another year if they like it, even if the policies aren't compliant with the Patient Protection and Affordable...
- Doi Moves To Allow Consumers To Continue Current Coverage Into 2014
The Illinois Department of Insurance (DOI) announced on November 22 that it will follow President Obama?s November 14 recommendation and allow insurance companies to renew a number of health plans in the individual and small group markets that do not...
