Health News
- As Nurse Practitioners Enjoy Their New, State-granted Authority, The Paducah Sun Looks At The Issue In Far Western Kentucky
Kentucky law has expanded the rights of nurse practitioners, Laurel Black notes for The Paducah Sun: "Local practitioners say the move will provide patients with better access to care, but not everyone in the medical community embraces the idea." The...
- Panel Of Physicians At National Conference Discuss Future Of Rural Primary Care, How To Solve Doctor Shortages
More needs to be done to address the shortage of primary-care physicians, a big problem in rural areas and much of Kentucky, according to a panel of physicians at "Rural Health Journalism 2014," Kris Hickman writes for the Association of Health Care...
- Family Physicians Group Objects To Cuts To Primary-care Physician Training Programs; Cites Doctor Shortage, Which Is Worse In Ky.
Facing an already-existing shortage of primary care in the country and state, the American Academy of Family Physicians sent a letter to U.S. Rep. Harold Rogers, R-Ky., chairman of the House Appropriations Committee, saying the committee's 2014...
- More Residency Placements Will Be Needed As Medical School Enrollments Rise, Perhaps By 30 Percent Through 2016
Aimed at addressing expected physician shortages, enrollment at U.S. medical schools is on target to increase by 30 percent by 2016, the Medical School Enrollment Survey has found. But even if enrollment rises through expansion of medical schools and...
- Intimacy After Menopause
It's no secret that "The Change" means change for you, your body and your partner. But life doesn't end after menopause - in fact, the best is yet to come! Dee-Dee Shiller, D.O., board-certified gynecologist and director of the new Women's...
Health News
Doctors of osteopathy are an increasing answer to the doctor shortage, as more osteopathic medical schools open
Doctors of osteopathy could be part of the solution to Kentucky's well-documented primary care doctor shortage, Laurel Black reports for The Paducah Sun.
"The American Association of Medical Colleges predicts that a growing population of aging people, health insurance expansion, and a freeze on Medicare funding for residency training positions will lead to a physician shortage of more than 90,000 by 2020," Black reports.
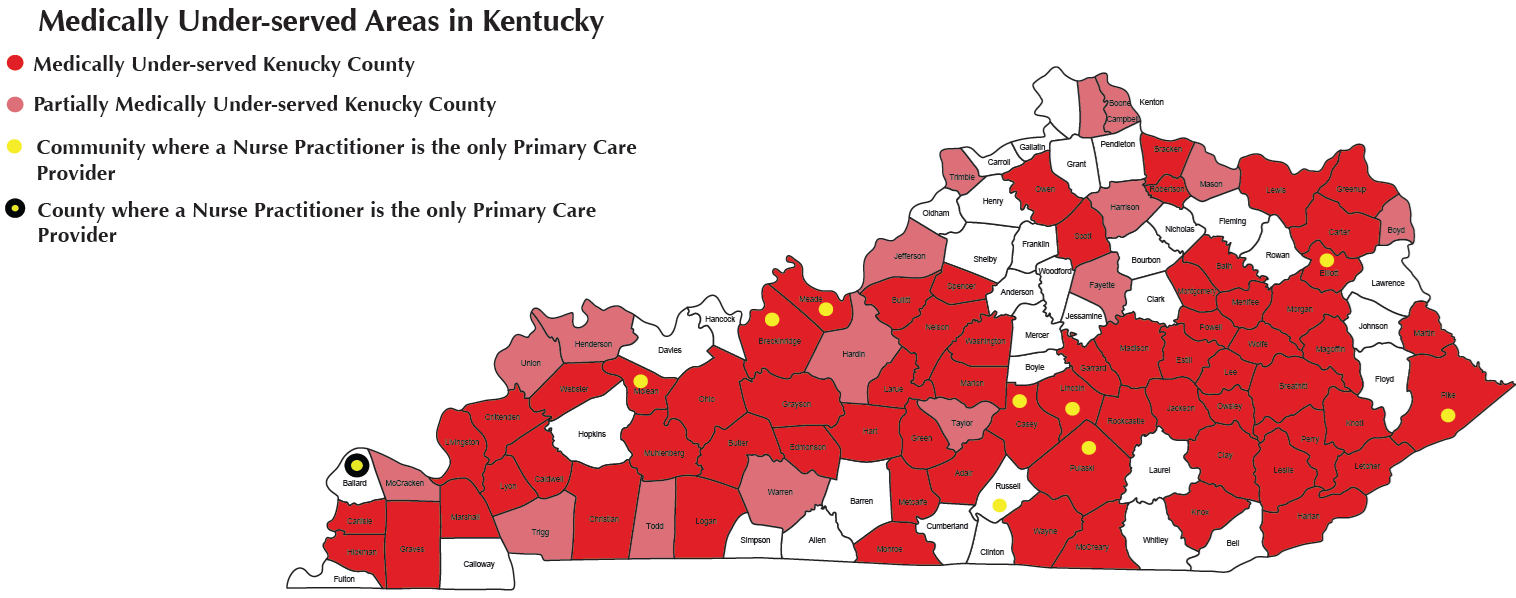
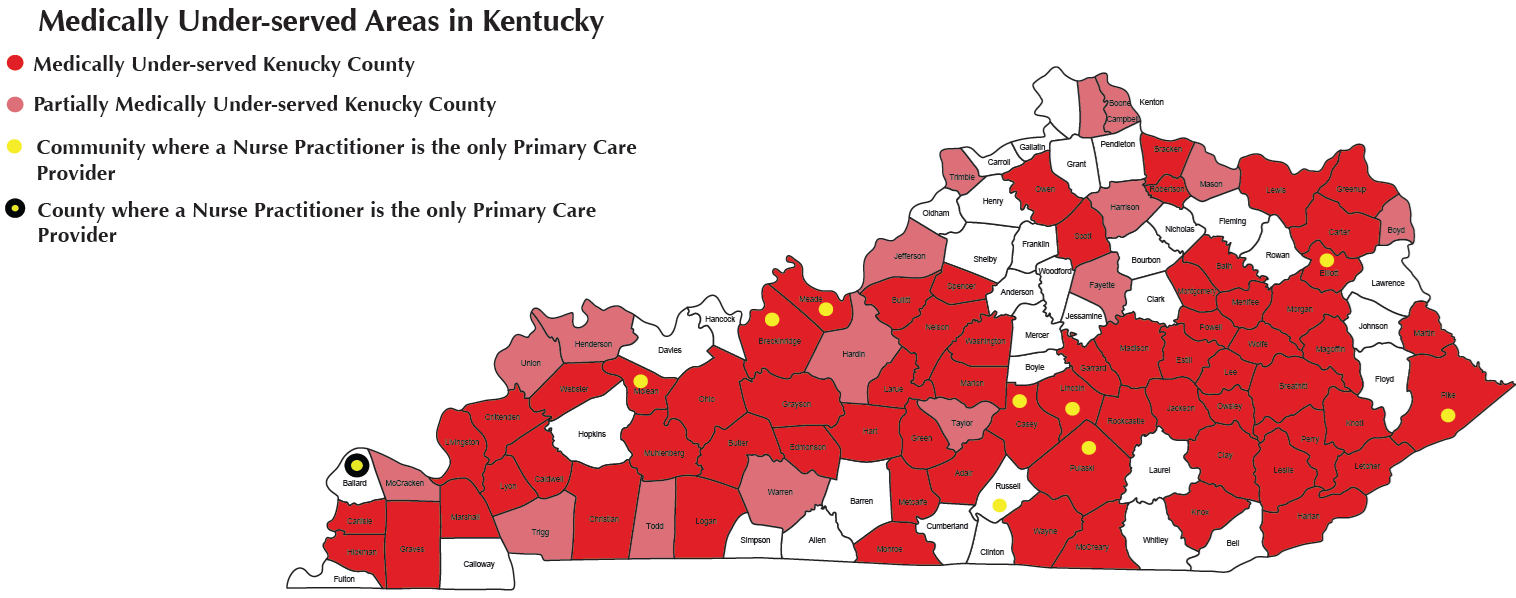
Rural areas are expected to be most affected by the shortage of physicians, especially in the area of primary care, Black writes. Kentucky is already experiencing this problem. A presentation at the 2013 Kentucky Rural Medical Educators Conference said Kentucky had a 1,287:1 primary care physician-to-citizen ratio, 557 short of the national average.
Despite this "looming doctor shortage," little attention has been given to osteopathic medicine as a possible solution, Black writes. But enrollment in osteopathic medicine, "which puts a focus on primary care and works to place its doctors in under-served regions," is growing.
"There are a lot of osteopathic schools. It's definitely a growing field," Griffin Bicking, a doctor of osteopathy and a vascular surgeon at Baptist Health Paducah, told Black.
"Graduates in osteopathic medicine have increased by more than 250 percent between 1980 and 2005, according to a study by the medical colleges' association. In 1980, there were 14 schools with fewer than 5,000 students in America; there are now 30 schools with more than 30,000 students," Black reports. "It's estimated that today nearly 30 percent of all medical school graduates are estimated to be doctors of osteopathy," or D.O.s.
The University of Pikeville's Kentucky College of Osteopathic Medicine has graduated more than 800 physicians since its inception in 1997, with 60 percent of these graduates serving primarily in rural healthcare facilities in Eastern Kentucky and other regions of Appalachia, according to its website.
New or relatively new osteopathic medical schools near Kentucky are in Harrogate, Tenn.; Lewisburg, West Virginia; and Blacksburg, Va. Other adjoining states with such schools include Ohio, Illinois, Indiana and Missouri.
Black reports that the stigma associated with D.O.s is fading as people seek a more holistic approach to their health. She also notes that the most notable difference between D.O.s and a doctor with traditional training is a required 300 to 500 hours of training in osteopathic manipulative treatment. This training, known as OMT, involves the movement of patient's bones and muscles to treat illness and injury and is part of the controversy surrounding D.O.s, Black reports.
However, more than half of D.O.s "used OMT on less than 5 percent of their patients," according to a study reported in Academic Medicine, the journal of the medical colleges' association, Black writes.
"Curriculum-wise, it's pretty much the same," Bradley Albertson, an internist and pediatrician at Mercy Primary Care in Benton, told Black of osteopathic medicine, which also requires four years of training followed by an internship and a residency. "The differences are more political and social."
Albertson opted for a non-osteopathic residency after attending a college of osteopathy for medical school, telling Black it "would add legitimacy to his practice."
And while osteopathic schools try to push primary care, D.O.s can go into any field a traditional doctor can, and it usually pays more to specialize, Black writes.
Albertson told Black that he is not sure that osteopathic schools will be the solution to the predicted patient-doctor gap and suggest it will take a "variety of solutions," including giving nurse practitioners more privileges.
"The American Association of Medical Colleges predicts that a growing population of aging people, health insurance expansion, and a freeze on Medicare funding for residency training positions will lead to a physician shortage of more than 90,000 by 2020," Black reports.
Rural areas are expected to be most affected by the shortage of physicians, especially in the area of primary care, Black writes. Kentucky is already experiencing this problem. A presentation at the 2013 Kentucky Rural Medical Educators Conference said Kentucky had a 1,287:1 primary care physician-to-citizen ratio, 557 short of the national average.
Despite this "looming doctor shortage," little attention has been given to osteopathic medicine as a possible solution, Black writes. But enrollment in osteopathic medicine, "which puts a focus on primary care and works to place its doctors in under-served regions," is growing.
"There are a lot of osteopathic schools. It's definitely a growing field," Griffin Bicking, a doctor of osteopathy and a vascular surgeon at Baptist Health Paducah, told Black.
"Graduates in osteopathic medicine have increased by more than 250 percent between 1980 and 2005, according to a study by the medical colleges' association. In 1980, there were 14 schools with fewer than 5,000 students in America; there are now 30 schools with more than 30,000 students," Black reports. "It's estimated that today nearly 30 percent of all medical school graduates are estimated to be doctors of osteopathy," or D.O.s.
The University of Pikeville's Kentucky College of Osteopathic Medicine has graduated more than 800 physicians since its inception in 1997, with 60 percent of these graduates serving primarily in rural healthcare facilities in Eastern Kentucky and other regions of Appalachia, according to its website.
New or relatively new osteopathic medical schools near Kentucky are in Harrogate, Tenn.; Lewisburg, West Virginia; and Blacksburg, Va. Other adjoining states with such schools include Ohio, Illinois, Indiana and Missouri.
Black reports that the stigma associated with D.O.s is fading as people seek a more holistic approach to their health. She also notes that the most notable difference between D.O.s and a doctor with traditional training is a required 300 to 500 hours of training in osteopathic manipulative treatment. This training, known as OMT, involves the movement of patient's bones and muscles to treat illness and injury and is part of the controversy surrounding D.O.s, Black reports.
However, more than half of D.O.s "used OMT on less than 5 percent of their patients," according to a study reported in Academic Medicine, the journal of the medical colleges' association, Black writes.
"Curriculum-wise, it's pretty much the same," Bradley Albertson, an internist and pediatrician at Mercy Primary Care in Benton, told Black of osteopathic medicine, which also requires four years of training followed by an internship and a residency. "The differences are more political and social."
Albertson opted for a non-osteopathic residency after attending a college of osteopathy for medical school, telling Black it "would add legitimacy to his practice."
And while osteopathic schools try to push primary care, D.O.s can go into any field a traditional doctor can, and it usually pays more to specialize, Black writes.
Albertson told Black that he is not sure that osteopathic schools will be the solution to the predicted patient-doctor gap and suggest it will take a "variety of solutions," including giving nurse practitioners more privileges.
- As Nurse Practitioners Enjoy Their New, State-granted Authority, The Paducah Sun Looks At The Issue In Far Western Kentucky
Kentucky law has expanded the rights of nurse practitioners, Laurel Black notes for The Paducah Sun: "Local practitioners say the move will provide patients with better access to care, but not everyone in the medical community embraces the idea." The...
- Panel Of Physicians At National Conference Discuss Future Of Rural Primary Care, How To Solve Doctor Shortages
More needs to be done to address the shortage of primary-care physicians, a big problem in rural areas and much of Kentucky, according to a panel of physicians at "Rural Health Journalism 2014," Kris Hickman writes for the Association of Health Care...
- Family Physicians Group Objects To Cuts To Primary-care Physician Training Programs; Cites Doctor Shortage, Which Is Worse In Ky.
Facing an already-existing shortage of primary care in the country and state, the American Academy of Family Physicians sent a letter to U.S. Rep. Harold Rogers, R-Ky., chairman of the House Appropriations Committee, saying the committee's 2014...
- More Residency Placements Will Be Needed As Medical School Enrollments Rise, Perhaps By 30 Percent Through 2016
Aimed at addressing expected physician shortages, enrollment at U.S. medical schools is on target to increase by 30 percent by 2016, the Medical School Enrollment Survey has found. But even if enrollment rises through expansion of medical schools and...
- Intimacy After Menopause
It's no secret that "The Change" means change for you, your body and your partner. But life doesn't end after menopause - in fact, the best is yet to come! Dee-Dee Shiller, D.O., board-certified gynecologist and director of the new Women's...
