Health News
- Consumer Reports Releases Annual Hospital-acquired Infection Report; Some Ky. Hospitals Have Work To Do; State To Get Data
A new study from Consumer Reports has analyzed hospital-acquired infection data for thousands of hospitals across the U.S. and rated them on how well they prevented these infections. Not all hospitals in Kentucky were rated, but of the ones that were,...
- Initial Research Is Promising For An Ancient Combination Of Natural Ingredients To Kill Mrsa, An Antibiotic-resistant Superbug
Researchers in England say an ancient folk cure might help kill the superbug MRSA, Justin Moyer reports for The Washington Post. MRSA, or methicillin-resistant Staphylococcus aureus, is among the infections that have grown resistant to antibiotics...
- Activist Seeking Stronger Rules On Reporting Health-care Infections Says Industry Lobbyists Misled Legislative Committee To Kill Bill
"Health-care industry witnesses appeared to have presented incorrect information" to the House Health and Welfare Committee in speaking March 6 against House Bill 460, which would require all health-care facilities to report infections associated with...
- Deadly, Drug-resistant Bacteria Are Becoming More Common In Kentucky Hospitals; Key Lawmaker Wants To Require Public Reporting
Nightmarish, drug-resistant bacteria that cause deadly infections are becoming more common in Kentucky hospitals, and a leading legislator on health issues says they should be required to report each case. The state Department for Public Health and hospital...
- How To Reduce Your Chance Of Aquiring A Staph Infection
In the news today, a new scientific report suggests that swimmers using public ocean beaches increase their risk for exposure to staph bacteria and potential infections. Staph infections are a growing public health concern. You acquire a staph infection...
Health News
Kentucky hospitals disagree on how to battle MRSA, an antibiotic-resistant and highly contagious bacteria that plagues them
Hospitals agree that precautions must be taken to fight the potentially deadly super bug MRSA, but they differ in their approaches, Laura Ungar reports for The Courier-Journal.
Ungar focuses on the Louisville Veterans Affairs Medical Center's screening approach to fight MRSA, the acronym for methicillin-resistant Staphylococcus aureus. Every patient is screened upon admission and when moved to another floor. The hospital also stresses hand washing, wearing gowns and gloves if a patient has MRSA, and continuing education on the issue.
The hospital began routine screening of the antibiotic-resistant and highly contagious bacteria in 2007 and says its infection rates have dropped 20 percent, falling to 0.09 infections per 1,000 days patients are in a hospital bed, compared with 1.89 infections per 1,000 in 2008, Ungar reports. A study of long-term-care facilities using this approach found a decrease in MRSA infections (36 percent over 42 months), according to an article in The American Journal of Infection Control.
?We don?t see many patients getting MRSA when they?re in the hospital anymore,? Dr. Raul Nakamatsu, an infectious disease physician at the Louisville VA Medical Center, said.
Some say more hospitals should follow the VA's lead. Dr. Kevin Kavanagh, chairman of Health Watch USA, and Lisa McGiffert, director of the Safe Patient Project at Consumers Union support this strategy. ?All hospitals should be doing this,? McGiffert told Ungar. ?It?s a strategy that?s proven to work.?
Other hospitals in the Louisville area screen only for high-risk patients, based on studies that encourage reducing MRSA with antibiotics and anti-infection cleansing cloths, Ungar reports. The cost of screening, which is about $55 per screening, is a concern, especially when hospitals consider other infection-control methods equally effective.
Those methods include emphasis on hand washing, isolating patients with MRSA, and wearing gowns and gloves while caring for them. Some hospitals only have private rooms, which they say decreases the chance of infection, and others wash high-risk patients with anti-infection cleansing or use antibiotics.
?In general, we have not done surveillance screening. It?s somewhat of a controversial topic,? Dr. Paul Schulz, an infectious disease specialist with Norton Healthcare, which promotes hand washing, isolation and wearing gowns and gloves to combat MRSA, told Ungar. ?We do all we can do that makes the most sense.?
The state only requires hospitals to report MRSA outbreaks, with no clear definition of what this means making it difficult to compare the two strategies, Ungar notes. No MRSA outbreaks in hospitals were reported in the state last year. The federal Centers for Disease Control and Prevention don?t require or recommend routine MRSA screening, although CDC does provide some guidelines on prevention strategies.
While people can carry MRSA without being infected, when an infection occurs, it causes serious skin, wound or blood infections, or pneumonia, which can be deadly, Ungar reports. Those most at risk are the chronically ill or those in hospitals or nursing homes. The Journal of the American Medical Association said there were more than 80,000 infections in 2011. The cost of treatment for severe MRSA infections can range from $20,000 into the millions, McGiffert told Ungar.
Five states now require screening of high-risk patients and although Kavanagh said that he thinks the chances are slim of Kentucky passing this law (a bill failed to pass in 2008) he would like to see it done voluntarily. ?If you have one facility that?s not doing a good job at controlling these infections,? he said, ?it can affect the whole community.?
Hospitals recognize that they must have a strategy to combat MRSA, but many have not found the need to move toward the aggressive screening procedures used by the VA. Those include the ALbert B. Chandler Medical Center at the University of Kentucky.
Dr. Derek Forster, medical director for infection prevention and control for UK HealthCare, told Ungar that the hospital keeps current on research and is willing to change strategies if it finds good evidence that one works much better than another: "We always keep an open mind."
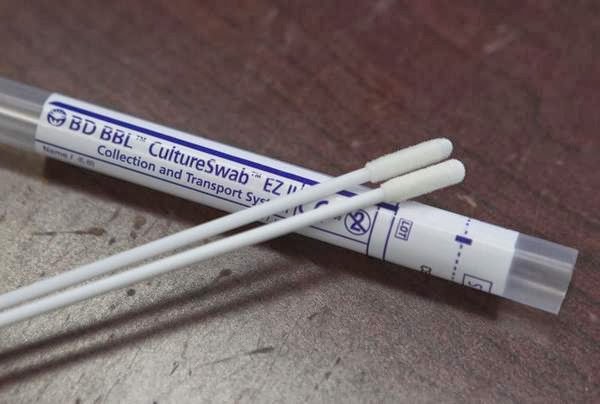 |
| Swab kits are used to screen for MRSA. (Photo: Matt Stone, C-J) |
The hospital began routine screening of the antibiotic-resistant and highly contagious bacteria in 2007 and says its infection rates have dropped 20 percent, falling to 0.09 infections per 1,000 days patients are in a hospital bed, compared with 1.89 infections per 1,000 in 2008, Ungar reports. A study of long-term-care facilities using this approach found a decrease in MRSA infections (36 percent over 42 months), according to an article in The American Journal of Infection Control.
?We don?t see many patients getting MRSA when they?re in the hospital anymore,? Dr. Raul Nakamatsu, an infectious disease physician at the Louisville VA Medical Center, said.
Some say more hospitals should follow the VA's lead. Dr. Kevin Kavanagh, chairman of Health Watch USA, and Lisa McGiffert, director of the Safe Patient Project at Consumers Union support this strategy. ?All hospitals should be doing this,? McGiffert told Ungar. ?It?s a strategy that?s proven to work.?
Other hospitals in the Louisville area screen only for high-risk patients, based on studies that encourage reducing MRSA with antibiotics and anti-infection cleansing cloths, Ungar reports. The cost of screening, which is about $55 per screening, is a concern, especially when hospitals consider other infection-control methods equally effective.
Those methods include emphasis on hand washing, isolating patients with MRSA, and wearing gowns and gloves while caring for them. Some hospitals only have private rooms, which they say decreases the chance of infection, and others wash high-risk patients with anti-infection cleansing or use antibiotics.
?In general, we have not done surveillance screening. It?s somewhat of a controversial topic,? Dr. Paul Schulz, an infectious disease specialist with Norton Healthcare, which promotes hand washing, isolation and wearing gowns and gloves to combat MRSA, told Ungar. ?We do all we can do that makes the most sense.?
The state only requires hospitals to report MRSA outbreaks, with no clear definition of what this means making it difficult to compare the two strategies, Ungar notes. No MRSA outbreaks in hospitals were reported in the state last year. The federal Centers for Disease Control and Prevention don?t require or recommend routine MRSA screening, although CDC does provide some guidelines on prevention strategies.
While people can carry MRSA without being infected, when an infection occurs, it causes serious skin, wound or blood infections, or pneumonia, which can be deadly, Ungar reports. Those most at risk are the chronically ill or those in hospitals or nursing homes. The Journal of the American Medical Association said there were more than 80,000 infections in 2011. The cost of treatment for severe MRSA infections can range from $20,000 into the millions, McGiffert told Ungar.
Five states now require screening of high-risk patients and although Kavanagh said that he thinks the chances are slim of Kentucky passing this law (a bill failed to pass in 2008) he would like to see it done voluntarily. ?If you have one facility that?s not doing a good job at controlling these infections,? he said, ?it can affect the whole community.?
Hospitals recognize that they must have a strategy to combat MRSA, but many have not found the need to move toward the aggressive screening procedures used by the VA. Those include the ALbert B. Chandler Medical Center at the University of Kentucky.
Dr. Derek Forster, medical director for infection prevention and control for UK HealthCare, told Ungar that the hospital keeps current on research and is willing to change strategies if it finds good evidence that one works much better than another: "We always keep an open mind."
- Consumer Reports Releases Annual Hospital-acquired Infection Report; Some Ky. Hospitals Have Work To Do; State To Get Data
A new study from Consumer Reports has analyzed hospital-acquired infection data for thousands of hospitals across the U.S. and rated them on how well they prevented these infections. Not all hospitals in Kentucky were rated, but of the ones that were,...
- Initial Research Is Promising For An Ancient Combination Of Natural Ingredients To Kill Mrsa, An Antibiotic-resistant Superbug
Researchers in England say an ancient folk cure might help kill the superbug MRSA, Justin Moyer reports for The Washington Post. MRSA, or methicillin-resistant Staphylococcus aureus, is among the infections that have grown resistant to antibiotics...
- Activist Seeking Stronger Rules On Reporting Health-care Infections Says Industry Lobbyists Misled Legislative Committee To Kill Bill
"Health-care industry witnesses appeared to have presented incorrect information" to the House Health and Welfare Committee in speaking March 6 against House Bill 460, which would require all health-care facilities to report infections associated with...
- Deadly, Drug-resistant Bacteria Are Becoming More Common In Kentucky Hospitals; Key Lawmaker Wants To Require Public Reporting
Nightmarish, drug-resistant bacteria that cause deadly infections are becoming more common in Kentucky hospitals, and a leading legislator on health issues says they should be required to report each case. The state Department for Public Health and hospital...
- How To Reduce Your Chance Of Aquiring A Staph Infection
In the news today, a new scientific report suggests that swimmers using public ocean beaches increase their risk for exposure to staph bacteria and potential infections. Staph infections are a growing public health concern. You acquire a staph infection...
